Pediatric Medulloblastomas
Pediatric Medulloblastomas
VI. Diagnosis
1. Clinical Features
Symptoms related to intracranial hypertension in younger children include behavioral problems, irritability, decreased interactivity, hypotonia and vomiting. When the fontanelles are still open, increase in head circumference is the predominant feature and may be associated with a bulging anterior fontanelle and gapping of sutures. However the fundus examination may be normal because of the possibility of the skull to expansion. In older children, headache, especially in the morning, dominates the picture.
Other revealing signs may point to the tumor such as vomiting without nausea occurring mainly in the morning. The vomiting sometimes is misinterpreted as a symptom of digestive ailments especially among younger children. Diplopia can result from cranial nerve six compression due to hydrocephalus. Visual disturbances are much rarer and are due to papilledema.
These signs may precede those related to cerebellar dysfunction for a time period which rarely exceeds two months. At a more advanced stage of intracranial hypertension, torticollis can occur suggestive of herniation of cerebellar tonsils into the foramen magnum necessitating an emergency hospitalization in neurosurgical unit.
2. Imaging Features
They aim to detect hydrocephalus, to better characterize the lesion for surgical resection and to search for any CNS metastases..
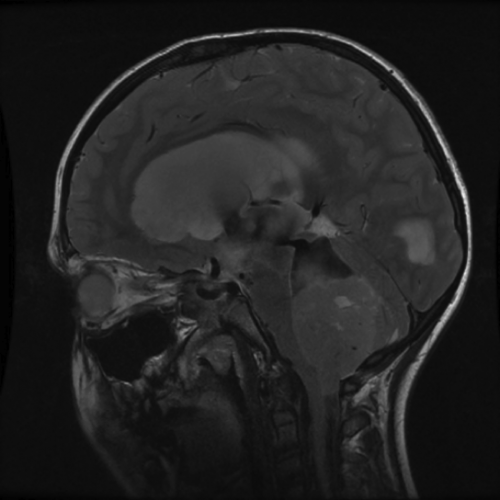
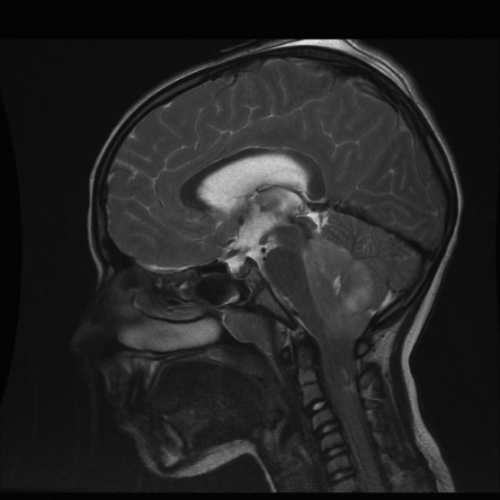
Brain MRI with and without contrast injection is the examination of choice. It precises on tumor location (usually the vermis with extension to the fourth ventricle, sometimes hemispheric or cerebellar pontine angle), its dimensions and its effects on the size of the ventricle. Typically, the MB is a rounded compact mass, at the center of the posterior fossa, homogeneous, hypointense relative to the cerebellar cortex in T1, iso-or hyperintense on proton density, hyperintense in T2, moderately enhanced after contrast medium injection. This classic form is observed in about half of cases. (Figures 1-5 and Figure 7). The diagnosis is more difficult when the tumor is invasive, necrotic, hemorrhagic, poorly enhancing, or when it extends to cerebellopontine angles.
Figure 1. Medulloblastoma: typical appearance: large tumor developing mainly into the fourth ventricle (Mid-Sagittal MRI T2-Weighted images). Note the radiological herniation of the lesion into the foramen magnum.
Figure 2. Paeditric Medulloblastoma: typical appearance. (Axial MRI T2-weighted Image showing a large fourth ventricular lesion).
Figure 3. Tumor growth into or towards the fourth ventricle, heterogeneous, seemingly well demarcated, with small cysts. (Axial MRI T2-weighted images).
Figure 4. Medulloblastoma: heterogeneous tumoral lesion, located in the fourth ventricle, with discrete and heterogeneous enhancement after gadolinium injection (axial cut of contrasted T1-weighted MRI image).
Figure 5. Mid-Sagittal MRI T2-weighted Image: endoscopic ventriculostomy permeability (flow artifact visible in the floor of the third ventricle). Large posterior fossa tumor.
Figure 7. Surgical emergency. Brain MRI: T2-weighted image Mid-Sagittal cut,. Voluminous posterior fossa lesion causing foramen magnum herniation and cranio-cervical junction compression.
The MRI sometimes allows for the appreciation of tumor infiltration of fourth ventricular, the brainstem, cerebellar peduncles and extension through the foramen of Lushka. It also enables detection of supratentorial and / or spinal metastases as well as meningeal dissemination in the form of contrast enhanced lesions of the arachnoid mater. MRI of the spinal axis should be complete, including the whole thecal sac. MRI is done preoperatively to avoid artifacts in the spine due to bleeding from surgery that can be mistaken for spinal “mets”. (Figures 1-8).

Figure 6. MRI : Mid-sagittal gadolinium-enhanced T1-weighted image. Nodular metastases along the spinal axis
Figure 8. Postoperative MRI with complete excision of the tumor.
3. Anatomopathologic Features (figure 11)
Figure 11. Classic medulloblastoma. Densely cellular lesion composed of cells with round or oval hyperchromatic nuclei and reduced cytoplasm, forming Homer Wright rosettes (hematoxylin and eosin, x400).
Diagnosis is based on histological examination of a non-necrotic tumor specimen. The diagnosis of medulloblastoma is made by the presence of small round or sometimes fusiform cells, which are very basophilic, with a high nucleo-cytoplasmic ratio, intense activity mitotic activity and sometimes arranged in the so called Homer-Wright rosettes or pseudorosettes, characterizing its neuroectodermal origin (24, 37).
The WHO 2007 classification (World Health Organization) places medulloblastoma under embryonic neuroepithelial tumors, and distinguishes them from other tumors of the same type located outside the cerebellum. Five histologic subtypes are distingished (37):
- The classic form composed of cells with hyperchromatic nuclei, and with less than 40% of Homer-Wright pseudo-rosettes.
- The desmoplastic / nodular type characterized by an abundance of collagen fibers and reticulin. Nodules correspond to zones of neuronal maturation. It occurs primarily in very young children in the cerebellar vermis but can also occur also in adolescents and young adults with cerebellar hemispheric localization. The prognosis is very good for young children (60).
- Two aggressive forms called anaplastic (5% of cases) and large cell medulloblastoma (2-4% of cases) have many similar features, including cells with large round and / or pleomorphic nuclei, vast bands of necrosis , a high mitotic index and a large proportion of cells in apoptosis. Their prognosis is pejorative (8).
- Medulloblastoma with extensive nodularity that occurs mostly in very young children
Other much more rare varieties, have been described: the medullomyoblastoma and melanotic medulloblastoma.
 Encyclopædia Neurochirurgica
Encyclopædia Neurochirurgica