 Brain arteriovenous malformation
Brain arteriovenous malformation
4.3. Radiosurgical treatment (Figure 13 and Figure 14)
Stereotactic radiosurgery can be used alone or together with embolization. It may also be used to treat small residual nidus after microsurgery. It is indicated mainly for patients in poor clinical conditions or with small lesions, deep or near eloquent areas. The complete obliteration takes from 1 to 3 years after the procedure. Obliteration rates for small AVMs (< 3 cm) is relatively high (from 81 to 90%), [20, 39, 43, 102], but less than half of the bigger lesions are effectively cured through radiosurgery, for grade IV lesions obliterations of the order of 20% are reported. [66] The obliteration rate of AVMs smaller than 4 ml is reported to be 85–100%, larger than 4 mL is reported to be 40–58%, and when it is larger than 10 ml both non-obliteration and complication rates rise with only a 32% obliteration. [21, 53, 81] When the volume is greater than 15 ml the obliteration rate decrease to 25% over a 40month period. [81]
Radiosurgery indication:![]() Patient prefer a non-invasive treatment and do not agree with neurosurgical intervention.
Patient prefer a non-invasive treatment and do not agree with neurosurgical intervention.![]() High surgical risk: due to AVM location or poor clinical condition.
High surgical risk: due to AVM location or poor clinical condition. ![]() Postoperative residual AVMs: mainly those located in deep cerebral areas.
Postoperative residual AVMs: mainly those located in deep cerebral areas.![]() AVMs located in deep cerebral areas: diencephalon, basal ganglia, internal capsule, and brain stem.
AVMs located in deep cerebral areas: diencephalon, basal ganglia, internal capsule, and brain stem.
Advantages are: avoids craniotomy and general anesthesia, allows the treatment of AVMs in deep locations or inaccessible with relatively low morbidity, low risk and no immediate discomfort.
Disadvantages are: complications vary and depend on the radiation dose. Headache, nausea and vomiting and seizures may occasionally happen. An important disadvantage is the time it takes for any curative effect to happen: two to three years; and during this period the risk of hemorrhage remains as for non-treated AVMs. Therefore, 8-10% of the patients bleed while waiting for the therapeutic effect of radiation (bleeding rate of 4% per year). Symptomatic edema caused by the radiation (radionecrosis) is another relevant complication related to the location of the AVM and to higher radiation doses, happening in about 10% of the cases [19]. Radionecrosis may result in focal neurological deficit or seizures; corticosteroids may help in the treatment, diminishing the sequel after several weeks or months. Transitory neurological worsening happens in approximately 5% of the cases and permanent neurological deficit may occur in 1.5 to 3% of the cases [57].
In the case of a large-volume AVM, radiosurgery (single dose) is associated with a significant risk of morbidity. Some strategies are used to reduce the risk of complication and try to increase the rate of obliteration as in staged-volume radiosurgery or hypofractionated stereotactic radiotherapy (also known as fractionated stereotactic radiosurgery).
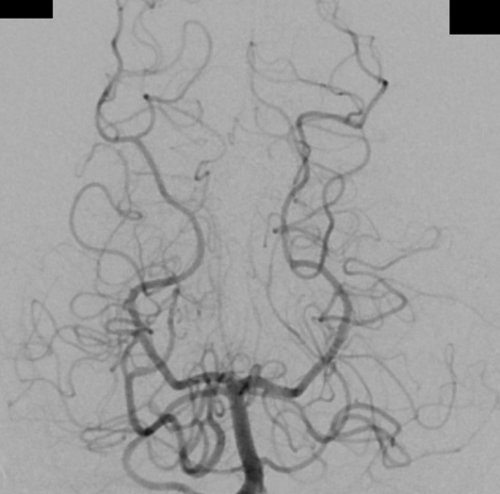
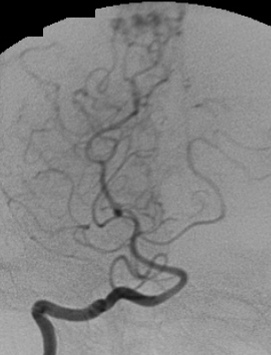
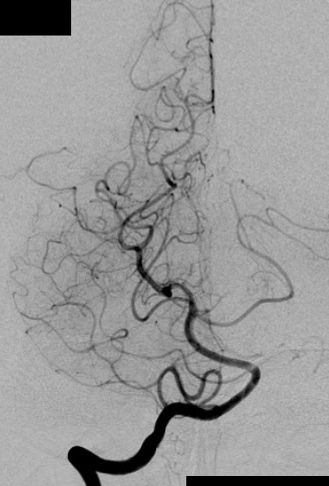
- Figure 13a
- Radiosurgical treatment. a) Angiography in a lateral projection of the right internal carotid artery showing an AVM fed by the right pericallosal artery.

- Figure 13b
- Radiosurgical treatment. b) Angiography in an AP projection of the right internal carotid artery showing an AVM fed by the right pericallosal artery.
- Figure 13c
- Radiosurgical treatment.
c) Angiography in an AP projection of the right vertebral artery showing an AVM fed by the right PCA.
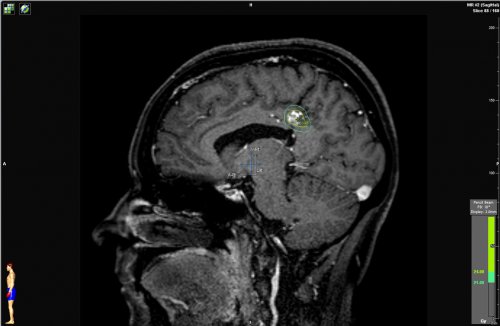
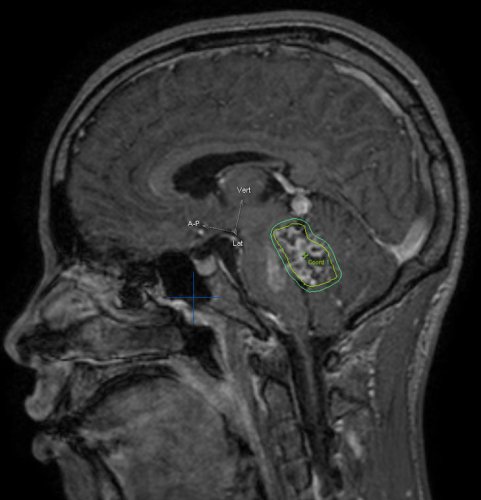
- Figure 13d
- Radiosurgical treatment.
d) Sagittal cerebral T1-weighted MRI with contrast showing an AVM at the posterior aspect of the cingulum gyrus. Observe the radiosurgical planning with a prescription dose of 24 Gy.
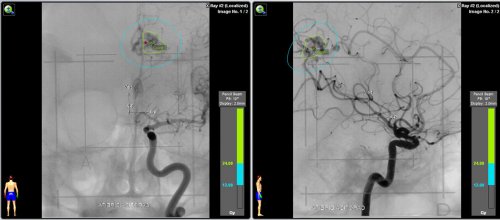
- Figure 13e
- Radiosurgical treatment.
e) Angiography in an AP and lateral projection of the right internal carotid artery showing the AVM and the planning with a prescription dose of 24 Gy.
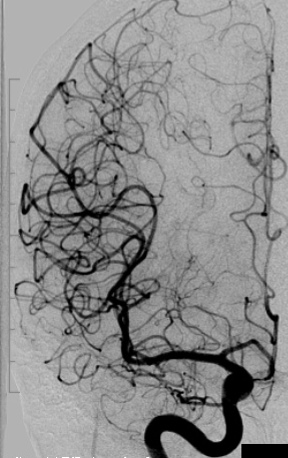
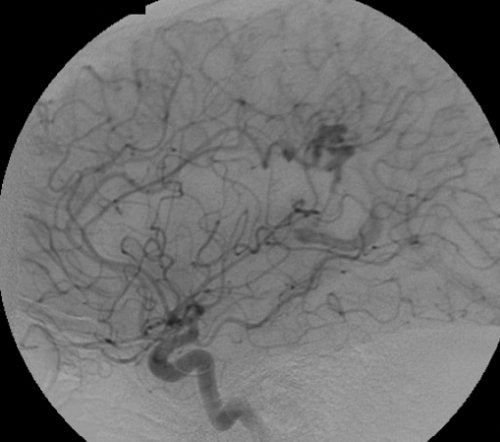
- Figure 13f
- Radiosurgical treatment.
f) Two years postoperative angiography of the right internal carotid artery in an AP projection showing complete occlusion of the AVM.

- Figure 13g
- Radiosurgical treatment.
g) Two years postoperative angiography of the right vertebral artery in a lateral projection showing complete occlusion of the AVM.
- Figure 13h
- Radiosurgical treatment.
h) Two years postoperative angiography of the right vertebral artery in an AP projection showing complete occlusion of the AVM.
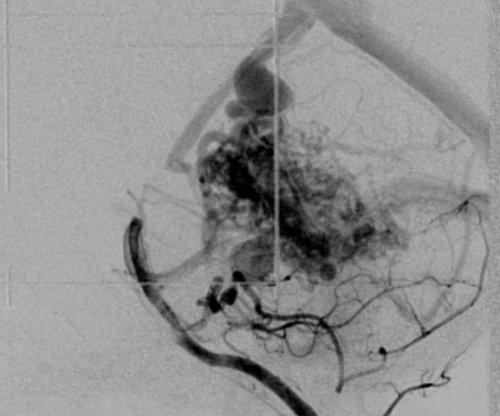
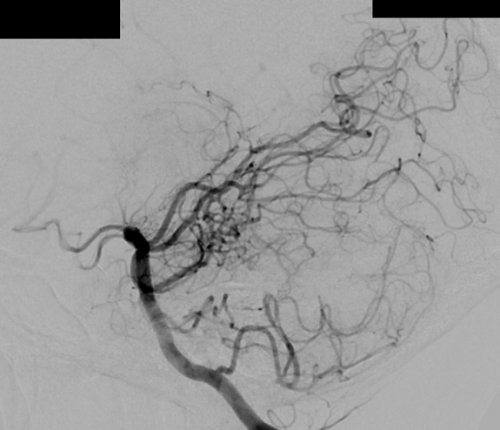
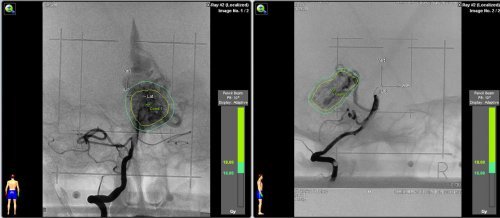
- Figure 14a
- Radiosurgical treatment. a) Angiography in a lateral projection of the left vertebral artery showing an AVM feed by the PCA and superior cerebellar artery.
- Figure 14b
- Radiosurgical treatment.
b) Angiography in an AP projection of the left vertebral artery showing an AVM fed by the PCA and superior cerebellar artery.
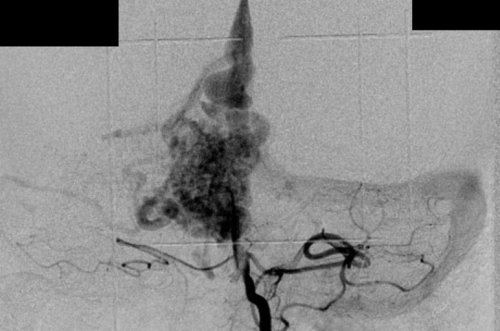
- Figure 14c
- Radiosurgical treatment.
c) Sagittal cerebral T1-weighted MRI with contrast showing an AVM inside the fouth ventricle. Observe the radiosurgical planning.
- Figure 14d
- Radiosurgical treatment.
d) Angiography in an AP and lateral projection of the right internal carotid artery showing the AVM and the planning with a prescription dose of 18 Gy.
 Encyclopædia Neurochirurgica
Encyclopædia Neurochirurgica