 Brain arteriovenous malformation
Brain arteriovenous malformation
*2. Imaging findings
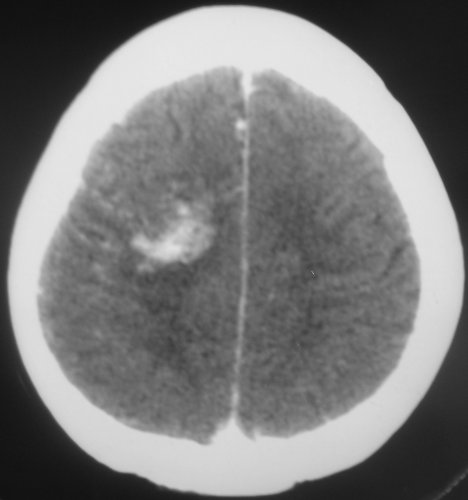
Radiological examinations are essential for the diagnosis of AVMs. ![]() Computed tomography (CT) is an excellent exam in emergency situations so as to identify acute hemorrhage (Figure 2). It is also useful to evaluate AVM calcification. In the CT, AVMs do not have any specific presentation, showing density similar to normal vessels, therefore a little denser than cerebral tissue and with high contrast enhancement, which helps to define the borders of the lesion. It can be difficult to detect an AVM through CT mainly when the nidus is smaller than 1 cm in diameter.
Computed tomography (CT) is an excellent exam in emergency situations so as to identify acute hemorrhage (Figure 2). It is also useful to evaluate AVM calcification. In the CT, AVMs do not have any specific presentation, showing density similar to normal vessels, therefore a little denser than cerebral tissue and with high contrast enhancement, which helps to define the borders of the lesion. It can be difficult to detect an AVM through CT mainly when the nidus is smaller than 1 cm in diameter.
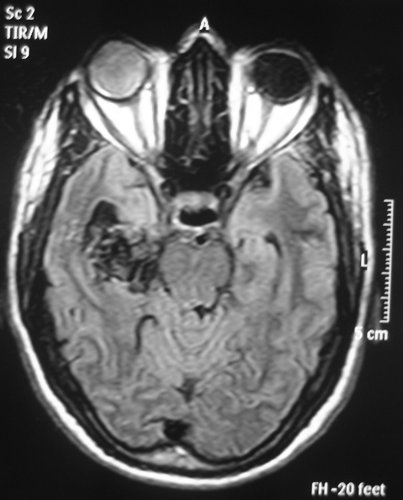
![]() Magnetic Resonance Imaging (MRI) is an excellent exam to diagnose AVMs allowing a three dimensional visualization of the lesion and thus helping to plan the surgical and radiosurgical treatment. For being constituted by countless vessels, AVMs show in MRI as flow voids in T1 and T2 weighted images and are enhanced by contrasts (Figure 3).
Magnetic Resonance Imaging (MRI) is an excellent exam to diagnose AVMs allowing a three dimensional visualization of the lesion and thus helping to plan the surgical and radiosurgical treatment. For being constituted by countless vessels, AVMs show in MRI as flow voids in T1 and T2 weighted images and are enhanced by contrasts (Figure 3).
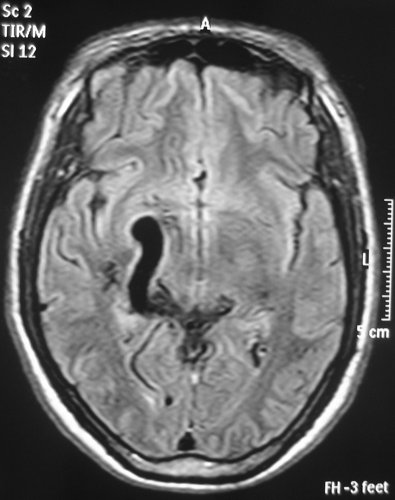
MRI also detects recent or old hematomas; and the Fluid-Attenuated Inversion-Recovery (FLAIR) sequence can show perinidal ischemic alterations, vasogenic edema or gliosis. A functional MRI (MRf) is also possible in order to relate the lesion to eloquent areas (motor, visual and speech).![]() Magnetic Resonance angiography (MRA) is useful in seeing the anatomy of the AVM in detail, showing details of its vessels. However it is not as good as digital angiography in the hemodynamic evaluation and for anatomic details, which are very important in treatment planning.
Magnetic Resonance angiography (MRA) is useful in seeing the anatomy of the AVM in detail, showing details of its vessels. However it is not as good as digital angiography in the hemodynamic evaluation and for anatomic details, which are very important in treatment planning.![]() Dynamic contrast-enhanced MRA is a promising non-invasive technique for studying AVMs. Images are acquired at multiple time points based on separation of the arterial, capillary, and venous phases of contrast passage to identify abnormal filling of the feeding arteries, nidus, and draining vessels of the AVM during the arterial phase. [72, 76, 88] Therefore the images produced are not static as in CTA or MRA, and may provide information about the hemodynamics of the AVMs. It produces high enough spatial and temporal resolution to enable us to visualize in detail the vascular architecture of the AVM. However, the detailed evaluation by conventional angiography is still the gold standard, because the current dynamic contrast-enhanced MRA does not yet have enough spatial and temporal resolution. [76]
Dynamic contrast-enhanced MRA is a promising non-invasive technique for studying AVMs. Images are acquired at multiple time points based on separation of the arterial, capillary, and venous phases of contrast passage to identify abnormal filling of the feeding arteries, nidus, and draining vessels of the AVM during the arterial phase. [72, 76, 88] Therefore the images produced are not static as in CTA or MRA, and may provide information about the hemodynamics of the AVMs. It produces high enough spatial and temporal resolution to enable us to visualize in detail the vascular architecture of the AVM. However, the detailed evaluation by conventional angiography is still the gold standard, because the current dynamic contrast-enhanced MRA does not yet have enough spatial and temporal resolution. [76]
Other benefits in relation to Computed Tomography Angiography (CTA) are the avoidance of radiation exposure, use of iodinated contrast material and in after intervention follow up, because clips and endovascular cast produces significant image artifacts in CTA. [72, 76]
![]() Computed Tomography Angiography (CTA) provides even more detailed information on the AVM vascularization than MRI, but less information on its relationship with brain parenchyma.
Computed Tomography Angiography (CTA) provides even more detailed information on the AVM vascularization than MRI, but less information on its relationship with brain parenchyma. ![]() Whole-brain CT angiography and perfusion combines dynamic 3-dimensional CT angiography of the brain with whole-brain CT perfusion imaging. [72, 80] It provides excellent spatial resolution, allows recognition of important AVM properties and may exhibit different pathologic phenomena, such as the arterial steal phenomenon and venous congestion. [72]
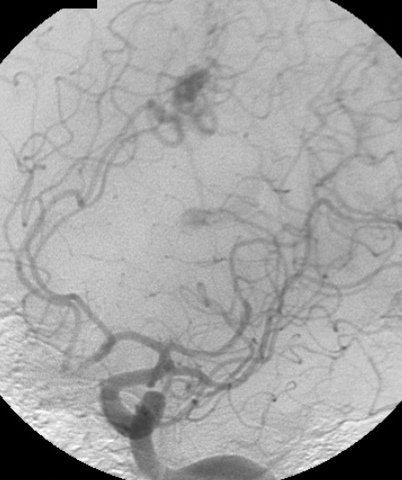
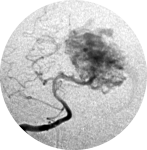
Whole-brain CT angiography and perfusion combines dynamic 3-dimensional CT angiography of the brain with whole-brain CT perfusion imaging. [72, 80] It provides excellent spatial resolution, allows recognition of important AVM properties and may exhibit different pathologic phenomena, such as the arterial steal phenomenon and venous congestion. [72]![]() Digital Subtraction Angiography (DSA) is the gold standard exam in the study of AVMs (Figure 4). It is necessary to analyze internal and external carotid arteries and vertebral arteries to learn about [87]:
Digital Subtraction Angiography (DSA) is the gold standard exam in the study of AVMs (Figure 4). It is necessary to analyze internal and external carotid arteries and vertebral arteries to learn about [87]:![]() The location and the real size of the nidus;
The location and the real size of the nidus;![]() The AVM arterial supply, including the deep and transventricular feeders;
The AVM arterial supply, including the deep and transventricular feeders;![]() Type of arteriovenous shunt (high versus low flow);
Type of arteriovenous shunt (high versus low flow);![]() Venous drainage pattern;
Venous drainage pattern;![]() Presence of aneurysms in the feeding arteries or intranidal aneurysms;
Presence of aneurysms in the feeding arteries or intranidal aneurysms;![]() Presence of venous stenosis, obstructions or abnormalities in the venous drainage;
Presence of venous stenosis, obstructions or abnormalities in the venous drainage;![]() Time distribution of arterial, parenchymatous and venous phases. The nidus is prematurely filled in the arterial phase due to the direct shunt from arteries to veins, making a type of bypass and making drainage veins tortuous and ectasic in response to the high blood flow and higher pressure.
Time distribution of arterial, parenchymatous and venous phases. The nidus is prematurely filled in the arterial phase due to the direct shunt from arteries to veins, making a type of bypass and making drainage veins tortuous and ectasic in response to the high blood flow and higher pressure.
One should keep in mind that in the case of small AVMs, when the initial manifestation is intracerebral hemorrhage, the hematoma might compress and hide the nidus, making the diagnosis through imaging difficult, even for MRI and DSA. Therefore, in such cases, when the first exams are negative for AVMs, they should be repeated after 4-6 weeks, after the reduction of hematoma mass effect.
Intraoperative angiography should be used to evaluate complete extirpation of the lesion. Unexpected residual AVM is shown in 3.7% to 27.3% of intraoperative digital subtraction angiograms after AVM resection cases. [13]
 Encyclopædia Neurochirurgica
Encyclopædia Neurochirurgica