 Brain arteriovenous malformation
Brain arteriovenous malformation
*2. Physiology
2.1. Pressure in feeding arteries
Smaller malformations (≤ 3 cm), because of greater vascular resistance, are supposed to be associated with a higher pressure in feeding arteries and, thus, have a greater chance probability of bleeding [77, 94]. However, this is a controversial hypothesis, because normally the small AVMs do not present epilepsy or flow steal phenomenon, and the only presentation is bleeding, and so a bias of presentation.
2.2. Venous contribution
According to some authors, anomalies in the venous components are predecessors of AVMs [68]. It is believed that, during the embryogenesis, anomalies in the cerebrovascular venous system may occur, such as venous occlusion, stenosis, or agenesis [67]. As time passes, factors such as venous hypertension end up transforming such anomalies into brain AVMs. Chronic venous hypertension raises intraluminal pressure, which may lead to the reduction of tissue perfusion and, then, ischemia [67], which releases chemical mediators that favor angiogenesis, besides diapedesis, that also favor angiogenesis if in excess by means of factors such as vascular endothelial growth factor (VEGF) [109]. Angiogenesis leads to the formation of arteriovenous fistulas, which cause an increase in the pressure of the venous bed, resulting in a vicious cycle that provokes the growth of AVMs.
Another theory is that the obstruction of venous drainage may cause the opening of pre-existing arteriovenous connections [109], thus leading to the formation of an AVM.
Some venous features are more highly subjected to bleeding, such as exclusively deep venous drainage, venous stenosis, and venous reflow [74]. On the other hand, arterial stenosis and arterial ectasia are not associated to a higher risk of bleeding.
2.3. Regulation of blood flow
AVMs are associated to the loss of blood flow regulation (impaired autoregulation), but it is not known if they cause it or result from it.
The “normal perfusion pressure breakthrough theory”, by Spetzler et al [97], advocates the possibility that auto-regulation is altered due to the AVM.
Other authors [68] say that auto-regulation changes are the cause for the growth and remodeling of AVMs, and may happen in a multi-factorial manner:![]() Arterial: high trans-nidal flow and arterial hypertension;
Arterial: high trans-nidal flow and arterial hypertension;![]() Venous: hypertension, thrombosis or stenosis;
Venous: hypertension, thrombosis or stenosis; ![]() Others: vascular lesion, abnormal endothelial signs, micro-shunt formation.
Others: vascular lesion, abnormal endothelial signs, micro-shunt formation.
2.4. AVM Structure
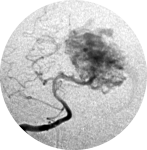
The structure of an AVM may range from really simple (Figure 1a), with a single compact nidus, one feeding artery and one or more draining veins, to very complex (Figure 1b), with multiple feeding arteries and draining veins, resulting in multiple nidus compartments, that can be contiguous or separated by a small amount of brain tissue, functional or not [68, 75, 113].

- Figure 01a
- The structure of an AVM may range from a) really simple, with a single compact nidus, one feeding artery and one or more draining veins.

- Figure 1b
- The structure of an AVM may range from b) very complex, with multiple feeding arteries and draining veins.
“Hidden compartments” can be present, showing as non-filled during angiography but in the follow-up may be filled and thus suggest AVM growth. Such compartments can be filled even after apparently complete AVM resection, thus suggesting a de novo AVM. ”Hidden compartments” can usually be identified through super-selective digital angiography [29].
The nidus can be:![]() Single: compact or diffuse (with one compartment);
Single: compact or diffuse (with one compartment);![]() Multiple: compact or diffuse (with more than one compartment).
Multiple: compact or diffuse (with more than one compartment).
2.5. Perinidal vessels
The terms “reserve nidus” and “perinidal dilated capillary network” refer to abnormal perinidal vessels that can be seen through angiography and that may later become part of the nidus [68, 90]. Due to the fact that perinidal vessels are connected to the nidus, it is believed that they are related to postoperative re-bleeding or de novo AVMs.
The terms “modja-modja” and “shaggy hair” are used to describe a hypervascular perinidal network. As they tend to bleed after nidal resection, it is advisable to coagulate these abnormal vessels, if present, during surgery and to induce hypotension in the postoperative course so as to lower the chances of re-bleeding and edema.
2.6. Flow steal
Brain AVMs are characterized by low resistance within the nidus secondary to the lack of an inter-posing capillary bed, thus depriving surrounding parenchyma of blood flow [115]. Flow steal caused by high flow arteriovenous shunt may be the cause of symptoms in some AVMs.
However there are controversies about its in vivo existence due to the disagreement regarding the several techniques that have been used to research it [68].
 Encyclopædia Neurochirurgica
Encyclopædia Neurochirurgica

