 Brain arteriovenous malformation
Brain arteriovenous malformation
*4. Therapeutic modalities
AVMs can be treated by microsurgical resection, endovascular embolization, or radiosurgery. Many times, it is necessary to use more than one modality of treatment to obtain the cure.
4.1. Surgical treatment
Surgical treatment has progressed considerably in recent years because of new microscopes, stereotactic guidance or neuronavigation, intraoperative electrophysiologic monitoring and intraoperative fluorescence video angiography using indocyanine green (ICG).
It is an elective procedure, when it presents with bleeding, surgery should usually be performed about two weeks after the ictus,that facilitates surgery. As observed by Lawton et al. [46] hematomas help separate AVMs from adjacent brain; evacuation of hematoma creates working space around the AVM that can minimize transgression of normal brain or access a deep nidus that might otherwise have been unreachable; and hemorrhage can obliterate some of the AVMs arterial supply to reduce its flow during resection. However when there is a voluminous intracerebral hematoma, causing intracranial hypertension that puts the life of the patient at risk, it is an emergency procedure. In such cases, an emergency drainage of the hematoma should be performed. However, if possible, a careful analysis based on CTA or DSA should take place in order to decide if it is possible to resect the nidus in the same surgery.
The complete excision of AVMs through microsurgery is still the treatment of choice in a great number of cases. (Figure 12)
Ideal AVMs to be treated by microsurgery are small (less than 3 cm in diameter) and symptomatic, located in non-eloquent areas.
Advantages are: immediate and permanent elimination of the risk of hemorrhage, improvement in neurological functions and reduction of seizure episodes [16, 34].
Disadvantages are: risks associated to craniotomy, general anesthesia, neurological deficits related to the surgery, and longer hospitalization when compared to other therapeutic options.
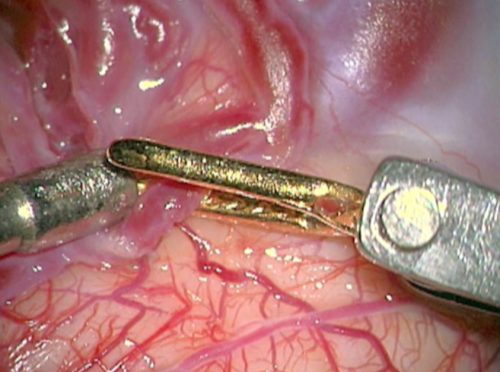
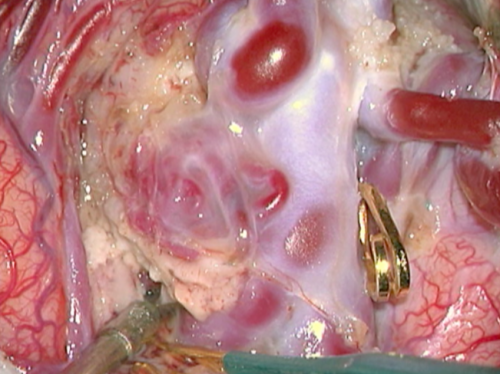
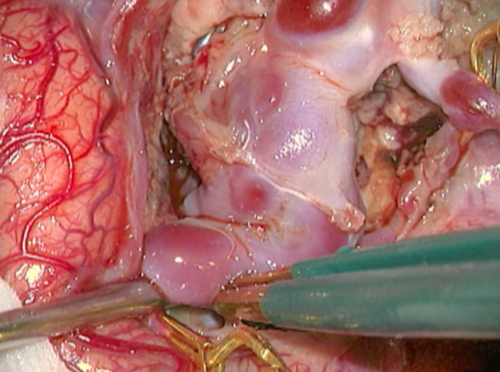
- Figure 12a Clipagem arteria nutridora 1
- Intraoperative nuances. a) and b) Clipping the feeding artery nearest to the nidus. a) Preparing to clip with a temporary clip.
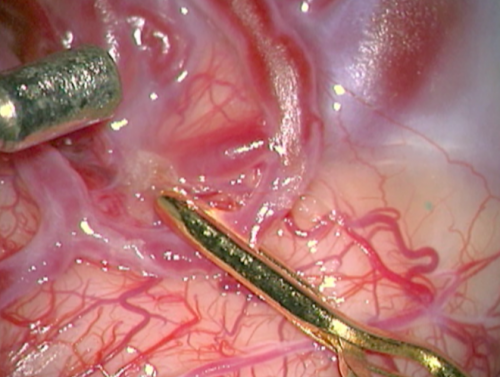
- Figure 12b Clipagem arteria nutridora 2
- Intraoperative nuances. a) and b) Clipping the feeding artery nearest to the nidus. b) The feeding artery is clipped and we can see a collapse between the clip and the nidus.
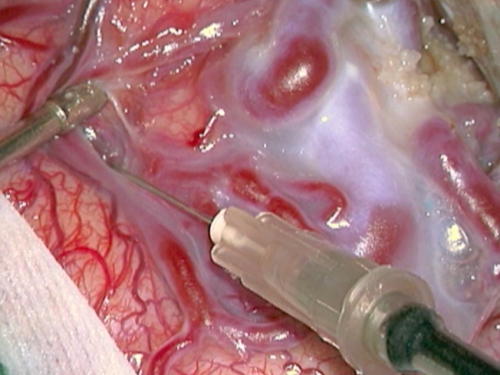
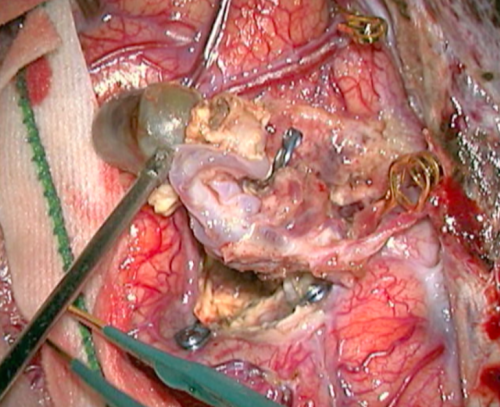
- Figure 12c Dissecção plano da MAV 1
- Intraoperative nuances. c) and d) Initial AVM dissection in its cleavage plane with the brain parenchima. c) Dissection with micro scalpel (insulin needle, 0,45 x 13mm).
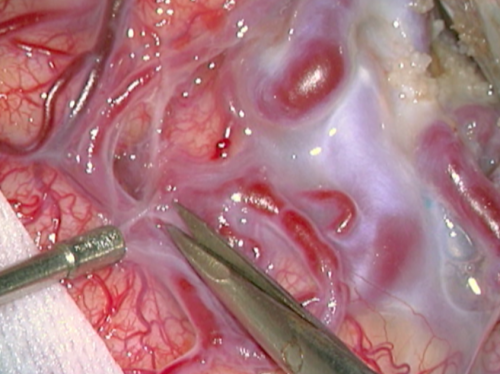
- Figure 12d Dissecção plano da MAV 2
- Intraoperative nuances. c) and d) Initial AVM dissection in its cleavage plane with the brain parenchima. d) Dissection with micro scissor.
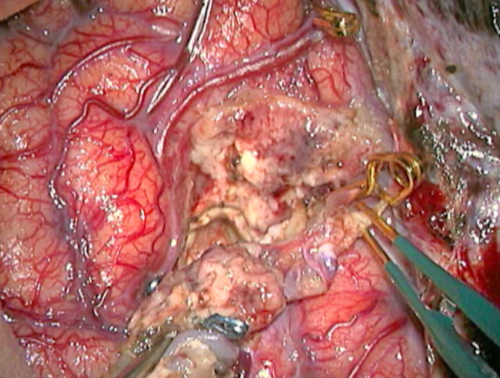
- Figure 12f Veia de drenagem inicial
- Intraoperative nuances. f) and g) Intraoperative images showing the nidus and draining vein aspects before and after the occlusion of the AVM nutrition. f) AVM with nidus and draining vein arterialized.
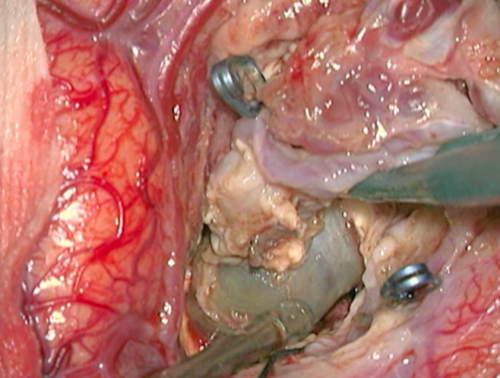
- Figure 12g Veia de drenagem após
- Intraoperative nuances. f) and g) Intraoperative images showing the nidus and draining vein aspects before and after the occlusion of the AVM nutrition. g) Change of the nidus and draining vein to dark blue after occlusion of the feeding branches.
 Encyclopædia Neurochirurgica
Encyclopædia Neurochirurgica